Trial at Jefferson shows new drug may help cancer patients who need stem cell transplants

A new drug may help cancer patients mobilize the cells necessary to restore their blood-forming system after high-dose chemotherapy, according to results from a clinical trial at the Kimmel Cancer Center at Thomas Jefferson University Hospital in Philadelphia and at other centers across the nation.
In the phase II trial, researchers were attempting to determine if patients with multiple myeloma or non-Hodgkin’s lymphoma who received the drug AMD-3100 along with the standard drug G-CSF (granulocyte-colony stimulating factor) would have more stem cells available for transplantation.
AMD-3100 blocks a specific cellular receptor, triggering the movement of stem cells out of the bone marrow and into the circulating blood, boosting the supply of marrow stem cells available for transplantation. Stem cell transplantation entails collecting certain types of cells known as hematopoietic stem cells from patients who receive treatment with high-dose radiation and/or chemotherapy for cancers such as leukemias, lymphomas and multiple myeloma, all of which involve the blood and immune system. The cells, once returned to the body, help restore the blood-forming system within the bone marrow – and the body’s immune system, which is severely damaged if not destroyed by treatment.
Stem cell transplantation is considered “front-line therapy for multiple myeloma, or cancer of the bone marrow, and for high-risk leukemia and lymphoma patients,” says Neal Flomenberg, M.D., professor of medicine and director of medical oncology at Jefferson Medical College of Thomas Jefferson University, who led the trial at Jefferson.
The researchers found that all of the 25 patients (10 patients with multiple myeloma and 15 patients with non-Hodgkin’s lymphoma) given the drug combination could move enough cells from the marrow to the bloodstream compared to only 64 percent of those who had G-CSF alone. They report their results September 1, 2005 in the journal Blood.
As a result, Dr. Flomenberg says, there were fewer stem cell collections necessary and more stem cells retrieved. The greater the number of available stem cells, the more likely transplantation will be successful. In some cases, this can mean the difference between a patient being able to receive a transplant or not. The drug has little toxicity.
“One of the most important results from the trial was that nine patients who would not have been able to mobilize stem cells to go to transplant with G-CSF alone could now mobilize them with the combination of G-CSF and AMD-3100,” Dr. Flomenberg says.
In addition, some patients who received AMD-3100 needed fewer stem cell collections to get the necessary number of cells, making the overall process less taxing. Those who still required the same number of collections had a higher total of stem cells.
“It’s hoped that the drug combination will make white cell and platelet recovery quicker and allow patients who wouldn’t have otherwise been able to mobilize stem cells for transplant now be able to do so,” he says. Without adequate numbers of stem cells for transplantation, patients may have a delayed recovery of their immune systems and be at greater risk of infection.
Most patients undergo standard chemotherapy for four to eight months before they have a stem cell transplant, he explains. Some patients won’t have a transplant until their disease relapses and treatment once again puts them back in remission. These treatments sometimes make subsequent stem cell collection difficult.
Approximately 25 percent to 35 percent of transplant patients – and perhaps as many as 65 percent – have trouble moving optimal numbers of stem cells from their bone marrow into the bloodstream using G-CSF. “Some patients with the standard approach don’t mobilize well, meaning more collections and often a poor or unusable cell product,” he says.
Dr. Flomenberg believes that the drug combination will become a standard treatment for such cases involving stem cell transplantation. “The treatment has potential to alter the standard of practice,” he says.
Researchers currently are conducting two phase III trials comparing G-CSF and placebo to G-CSF and AMD-3100 in 600 patients with either non-Hodgkin’s lymphoma or multiple myeloma, he notes. Jefferson is participating in both trials, in addition to another phase II trial with AMD-3100 alone.
The research is sponsored by AnorMED, Inc., a Vancouver, British Columbia-based drug development company. AnorMED’s efforts are aimed at the discovery and development of small molecule therapeutics to treat diseases including HIV, rheumatoid arthritis, asthma and cancer.
Media Contact
More Information:
http://www.jefferson.eduAll latest news from the category: Life Sciences and Chemistry
Articles and reports from the Life Sciences and chemistry area deal with applied and basic research into modern biology, chemistry and human medicine.
Valuable information can be found on a range of life sciences fields including bacteriology, biochemistry, bionics, bioinformatics, biophysics, biotechnology, genetics, geobotany, human biology, marine biology, microbiology, molecular biology, cellular biology, zoology, bioinorganic chemistry, microchemistry and environmental chemistry.
Newest articles
Advance in light-based computing
…shows capabilities for future smart cameras. UCLA-developed experimental device demonstrates ability to reduce glare in images. Researchers developing the next generation of computing technology aim to bring some light to…
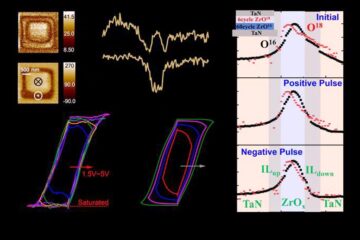
Evidence for reversible oxygen ion movement during electrical pulsing
…enabler of the emerging ferroelectricity in binary oxides. In a recent study published in Materials Futures, researchers have uncovered a pivotal mechanism driving the emergence of ferroelectricity in binary oxides….

Next-generation treatments hitch a ride into cancer cells
Researchers from Osaka University discover that opening a channel into cancer cells helps antisense oligonucleotide drugs reach their targets. Antisense oligonucleotides (ASOs) are next-generation drugs that can treat disease by…





















