How HIV disables the cells’ call for help

Weizmann Institute Scientists discover how an HIV protein fragment shuts down an immune response. Their finding may have implications for autoimmune disease treatment.
The HIV virus hides out in the very immune system cells that are meant to protect the body from viral infection. But how does it prevent these cells from mounting a full-scale attack against the invader? In research published today in the Journal of Clinical Investigation, a team at the Weizmann Institute of Science has shown how a part of a protein on the virus’ outer surface interferes with the cells’ normal immune response. But their work may have wider implications: this molecular fragment, which has such a devastating effect in one disease, might turn out to be an effective treatment for other disorders such as rheumatoid arthritis.
In the initial stages of HIV infection, the protein coatings of the viruses fuse with the outer membranes of T cells – immune system cells that recognize foreign invaders and alert other types of immune cell to come to the rescue. The genetic material of the virus, which is basically a strand of RNA, then forces the cell’s DNA to make copies of it. Newly minted viruses created by the host DNA later break out of the cell membrane to infect other cells. Many believed that the very act of breaking into T cells and hijacking their DNA was enough to destroy the ability of these cells to call up immune support.
But Institute scientists Prof. Yechiel Shai of the Biological Chemistry Department, Prof. Irun Cohen of the Immunology Department and graduate students Francisco Quintana and Doron Gerber thought there must be more to the story. T cells identify invaders using receptors, like security antennae, on their outer walls. A virus, especially one with its own surface equipment for seeking out specific T cells, would be hard-pressed to slip past these receptors without raising the alarm. The scientists surmised that the virus must be able to actively disable some part of the immune cell’s system.
They investigated a peptide fragment called FP (fusion peptide), a segment of the HIV protein gp41 found on the viral envelop. FP was known to play a role in the complex process in which the viral envelop fuses with the cell membrane in the initial stage of cell infection. The researchers suspected that FP, which is only exposed for a short period during this process, may have enough time to affect the immune response as well. Indeed, they found that FP locks on to several proteins on the cell walls that are involved in invoking a large-scale immune response, effectively shutting them down.
From their new understanding of how a tiny virus can gain control of the body’s immune response, the scientists made an intuitive leap. In autoimmune diseases, the same T cells that play host to HIV viruses are overactive, mistakenly attacking the body’s cells instead of foreign invaders. If the viruses use FPs to override the cells’ call for help, could their actions, which block one type of immune response without killing the cell, be applied to these autoimmune diseases? To check their theory, the research team tested FP on rats suffering from an autoimmune syndrome similar to human rheumatoid arthritis, and on cultured human T cells. As they predicted, the rats treated with FP showed a significant reduction in joint swelling and other symptoms of arthritis.
Shai points out that using FP, a tiny piece of a piece of the HIV virus, would pose no danger to patients as it lacks any ability to either infect cells or to reproduce. Rather, as the scientists note in their paper, the study of a destructive virus may contain important lessons on how to regulate the immune system. “Perhaps,” says Cohen, “we humans can adopt the virus peptide to better control overactive autoimmunity.”
Prof. Irun Cohen’s research is supported by the Minna James Heineman Stiftung; the Robert Koch Minerva Center for Research in Autoimmune Disease; and Mr. and Mrs. Samuel Theodore Cohen, Chicago, IL.
Prof. Cohen is the incumbent of the Helen and Morris Mauerberger Professorial Chair in Immunology.
Prof. Yechiel Shai’s research is supported by Robert Koch Minerva Center for Research in Autoimmune Disease; and the estate of Julius and Hanna Rosen.
Prof. Shai is the incumbent of the Harold S. and Harriet B. Brady Professorial Chair in Cancer Research.
Media Contact
All latest news from the category: Life Sciences and Chemistry
Articles and reports from the Life Sciences and chemistry area deal with applied and basic research into modern biology, chemistry and human medicine.
Valuable information can be found on a range of life sciences fields including bacteriology, biochemistry, bionics, bioinformatics, biophysics, biotechnology, genetics, geobotany, human biology, marine biology, microbiology, molecular biology, cellular biology, zoology, bioinorganic chemistry, microchemistry and environmental chemistry.
Newest articles
High-energy-density aqueous battery based on halogen multi-electron transfer
Traditional non-aqueous lithium-ion batteries have a high energy density, but their safety is compromised due to the flammable organic electrolytes they utilize. Aqueous batteries use water as the solvent for…

First-ever combined heart pump and pig kidney transplant
…gives new hope to patient with terminal illness. Surgeons at NYU Langone Health performed the first-ever combined mechanical heart pump and gene-edited pig kidney transplant surgery in a 54-year-old woman…
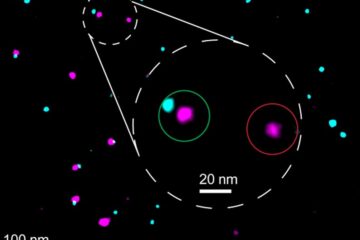
Biophysics: Testing how well biomarkers work
LMU researchers have developed a method to determine how reliably target proteins can be labeled using super-resolution fluorescence microscopy. Modern microscopy techniques make it possible to examine the inner workings…





















