Herceptin Backgrounder

It was the first of the new-generation targeted therapies, and, in some ways, it remains the standard bearer. More women with breast cancer are treated with Herceptin, which was approved for use in 1998 after decades of development, than are patients using the newer targeted drugs that treat other cancers.
Herceptin can strike the most aggressive breast cancer that has spread with an effectiveness no chemotherapy agent has yet matched. And such help is much needed. Breast cancer is the most common cancer diagnosed in women, and despite improvements in traditional treatment, up to half of breast cancer patients develop cancer that has spread, or that keeps coming back — leading to 40,000 deaths a year. Herceptin, which can be used in 25 percent to 30 percent of those patients, has managed to make a dent in those statistics.
But like other tailored drugs that attack only cancer cells, Herceptin can often fail patients. Many patients do not respond to Herceptin, and in most who do, the cancer begins to grow again within a year, leaving few available treatment options.
Researchers at The University of Texas M. D. Anderson Cancer Center are determined to understand why patients who should be helped by the drug aren’t, and why tumors that once disappeared due to Herceptin treatment can become “resistant” to the drug. They are, in short, searching for ways to increase the magnitude and duration of response to the agent — to tweak a good drug into a great one.
“Herceptin is one of the best tools that we have for treating HER-2-positive metastatic breast cancer, but it is not as effective as we would like it to be,” says Francisco J. Esteva, M.D., an associate professor in the Department of Breast Medical Oncology who is leading an effort to define and improve the drug’s biological action. “There are areas, however, where we think it can be improved.”
Investigations at M. D. Anderson to understand and perfect Herceptin involve both basic research work and clinical investigation. For example, basic researchers are finding clues as to how Herceptin confers resistance, and in the clinical arena, they have found that use of the drug in earlier stages of breast cancer appears to offer the best response — a major advance that could help thousands of women.
“Herceptin is already changing the natural course of breast cancer, but we believe there is much more that it can do,” says Aman Buzdar, M.D., a professor in the Department of Breast Medical Oncology who has found a promising new use of the drug. “We are finding out when it works, why it works and why it doesn’t.”
Maximizing a new breed of drug
Herceptin was born when scientists began to use the new tools of molecular biology to find genes that seemed to be associated with particular cancers. The first breakthrough occurred decades ago when researchers discovered a gene, dubbed neu, that seemed to cause breast cancer in rats. In the 1980s, the human equivalent to the rat gene, its “homolog,” was identified and named her-2 (for human epidermal growth factor receptor 2). Soon after its discovery, scientist Dennis Slamon, M.D., Ph.D., at the University of California, Los Angeles, reported that women whose breast cancer had more copies of the her-2 gene spread the fastest, resulting in a poor prognosis. Patients with the her-2 alteration relapse more quickly and die more often than those patients whose breast cancer cells have normal her-2 function.
Her-2 is part of a family of genes (her-1 through her-4) that play a role in regulating growth in a cell. Like all genes, her-2 does this by ordering production of proteins that sit on the outside of the cell body, like little antennas, waiting for other protein “signals” that set off a chain reaction, telling the cell to grow and not to die in the process. This can be part of a normal cell cycle. But when the her-2 gene is amplified and overly active — for reasons that are not understood — it studs a cell with too many receptors, proteins referred to as HER-2, causing the cell to grow uncontrollably. A typical breast cell has 50,000 HER-2 receptors on its surface; a breast cancer cell can have as many as 1.5 million such antennae.
At first, Slamon and others thought they could use this knowledge to test patients to see if they had such an aggressive cancer. It turned out that 25 percent to 30 percent of breast cancers over-express HER-2, and are more likely to grow fast, come back, spread to other organs and be difficult to treat. The researchers then reasoned that if they could design an agent that blocked HER-2 receptors, that growth signal would be shut down.
Herceptin, produced by the biotech company Genentech, does that; it is made up of large antibody molecules that smother and disable the receptor and also alert the immune system to selectively destroy the tumor cells. Clinical tests that led to the drug’s approval showed that women with metastatic cancer that over-produces HER-2 who used Herceptin with chemotherapy experienced a 24 percent increase in median overall survival, or almost five months, compared with women treated with chemotherapy alone. That advance cut the one-year death rate from 33 percent to 22 percent in women who responded. However, the drug did not help the majority of patients in the trial, even though their tumors over-expressed HER-2.
Herceptin became the first of the new breed of drugs targeted only at cancer cells. Because it doesn’t usually attach to other types of proteins, Herceptin rarely cripples normal cells, compared to chemotherapy, which affects all cells that grow and divide. And unlike standard chemotherapy, Herceptin can be taken indefinitely to keep the breast cancer under control, as long as side efects such as the heart damage that has been associated with the drug doesn’t occur.
Clinicians at M. D. Anderson conducted some of the initial studies proving the drug could work in metastatic breast cancer, and they also participated in the large clinical trials that led to approval of the drug for treatment of metastatic breast cancer. But the institution is mostly making its mark on Herceptin by looking at how to improve use of the drug.
Researchers at M. D. Anderson have launched studies to understand what kind of patients would benefit most from the drug, and they are testing some new ideas about how Herceptin can work best in cancer that has spread.
For example, they found that while over-expression of HER-2 increases resistance to the chemotherapy drug Taxol, use of Herceptin improved the effectiveness of Taxol. Clinicians at M. D. Anderson also are testing Herceptin in combination with other chemotherapy agents as well as with non-traditional drugs such as other targeted therapies, which have led to evidence of improved life span. They also are looking at the effect of using different doses of Herceptin as well as different dosing schedules, and are working on a blood test that can predict Herceptin’s effectiveness in individual patients.
But, according to Esteva, some of M. D. Anderson’s most important clinical work to date with Herceptin “is trying to learn how to use the drug to treat early-stage breast cancer.”
The fruits of such ongoing work were realized earlier this year when Buzdar presented results of a small study at the annual meeting of the American Society of Clinical Oncology. Results from a clinical trial testing use of Herceptin in early-stage HER-2 positive breast cancer were so strong that the study was halted early so that all newly diagnosed patients at M. D. Anderson could benefit from the treatment.
Buzdar and his team found that when Herceptin was used along with pre-surgery chemotherapy, twice as many breast tumors had disappeared at the time of surgery, compared to use of chemotherapy alone. In the 42-patient study, more than 65 percent of patients with early-stage, HER-2-positive breast cancers experienced a complete response (no cancer left in the breast or in the lymph nodes at the time of surgery) after receiving Herceptin with chemotherapy, compared to 26 percent of patients with similar tumor types who received chemotherapy by itself before surgery.
When he began the study more than two years ago, Buzdar had hoped to see a 20 percent improvement in complete response rate — but the actual improvement was 39 percent. That may be because both treatments were working together to block the multiple roadways that cancer cells can take to grow. “There was a lot of synergism between Herceptin and chemotherapy in this trial. One plus one became five,” says Buzdar. “In my 30-plus years of clinical research in breast cancer, I believe these are among the most striking results I have seen.”
The research team is using experience gained from the trial to develop future studies in a larger group of patients, he says. They are also building on data collected in the three decades that M. D. Anderson has pioneered use of neoadjuvant chemotherapy (chemotherapy before surgery) in different cancer types. “We know from experience that if we eradicate the cancer before surgery, close to 90 percent of patients remain disease free.”
“Drugs often show their maximum potential in early-stage disease, and this also appears to be true for Herceptin,” says Buzdar. “It helps some patients with metastatic breast cancer, but it may be able to eradicate a much higher proportion of cancer in patients with earlier disease.”
Understanding its secrets
Even while clinicians at M. D. Anderson are working to maximize the potential of Herceptin treatment, researchers in the lab are striving to understand why it works and how it fails.
Unlocking the secrets of both Herceptin and the HER-2 pathway will help tens of thousands of patients – the three out of every 10 women diagnosed with this particularly stubborn and deadly cancer, says Gabriel Hortobagyi, M.D., a professor and chairman in the Department of Breast Medical Oncology. “HER-2 has become an important target for the development of novel therapies that exploit our growing understanding of the molecular mechanisms that mediate carcinogenesis and metastasis,” he says.
Several research teams at M. D. Anderson are focusing, in particular, on why cancer cells are either initially resistant to Herceptin, or become resistant over time, says Esteva. Such findings could improve Herceptin therapy, he says: “If resistance occurs in a specific pathway, then it may be possible to introduce an agent that can reverse that resistance.”
For example, the study by Dihua Yu, M.D., published August 2004 in the journal Cancer Cell (see associated news release) potentially explains why some patients with HER-2-positive tumors never respond to Herceptin. The finding that presence of a protein known as PTEN, which helps put a brake on cancer growth, determines whether or not Herceptin will work suggests that PTEN can become a powerful predictor of who will respond to Herceptin. It also implies that drugs that mimic the action of PTEN could help restore Herceptin’s beneficial effects.
Esteva has also found another pathway that might be targeted to restore Herceptin sensitivity. Results published by his laboratory June 1, 2004 in the journal Cancer Research showed that Herceptin-resistant cells lost p27kip1, a molecule that can arrest cell growth. “This is another pathway that we can target to restore the ability of Herceptin to treat breast cancer,” he says.
But progress is slow in the effort to tease apart the “complex story” of Herceptin resistance, he says. “There is not one simple pathway by which cancer cells promote their growth, but these pathways talk to each other,” Esteva says, “so the goal is to find those molecules responsible for prolonging Herceptin’s effectiveness.”
Researchers are using genomics and proteomics to look at all the genes involved in HER-2-positive tumors, “but we are at the caveman stage in our understanding of all the mechanisms involved,” Esteva says. “Still, Herceptin provides the proof of principle that targeting specific receptors can result in clinical benefit, and now we are building upon that new research plateau.” Written by: Renee Twombly
Media Contact
More Information:
http://www.mdanderson.orgAll latest news from the category: Life Sciences and Chemistry
Articles and reports from the Life Sciences and chemistry area deal with applied and basic research into modern biology, chemistry and human medicine.
Valuable information can be found on a range of life sciences fields including bacteriology, biochemistry, bionics, bioinformatics, biophysics, biotechnology, genetics, geobotany, human biology, marine biology, microbiology, molecular biology, cellular biology, zoology, bioinorganic chemistry, microchemistry and environmental chemistry.
Newest articles

Properties of new materials for microchips
… can now be measured well. Reseachers of Delft University of Technology demonstrated measuring performance properties of ultrathin silicon membranes. Making ever smaller and more powerful chips requires new ultrathin…

Floating solar’s potential
… to support sustainable development by addressing climate, water, and energy goals holistically. A new study published this week in Nature Energy raises the potential for floating solar photovoltaics (FPV)…
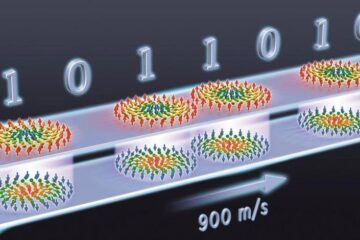
Skyrmions move at record speeds
… a step towards the computing of the future. An international research team led by scientists from the CNRS1 has discovered that the magnetic nanobubbles2 known as skyrmions can be…





















