Penn Study Gives Hope for New Class of Alzheimer’s Disease Drugs

A new Penn study, published this week in the Journal of Neuroscience, has found and tested in an animal model of Alzheimer’s disease a class of drug that is able to enter the brain, where it stabilizes degenerating neurons and improves memory and learning.
In the normal brain, the protein tau plays an important role in stabilizing structures called microtubules in nerve cells, which serve as tracks upon which cellular material is transported. In Alzheimer’s disease and related disorders, tau becomes insoluble and forms clumps in the brain. One consequence of these aggregates is a depletion of normal tau, resulting in destabilization of the microtubule tracks that are critical for proper nerve-cell function.
Senior authors Virginia M.-Y. Lee, PhD, director of the Center for Neurodegenerative Disease Research (CNDR), and John Trojanowski, MD, PhD, director of the Institute on Aging and CNDR co-director, introduced the concept of using microtubule-stabilizing drugs over 15 years ago to counteract tangles of tau and compensate for the loss of normal tau function. Kurt Brunden, PhD, director of Drug Discovery at CNDR and Bin Zhang, MD, PhD, senior research investigator, are the first authors on this study from the University of Pennsylvania School of Medicineand the School of Arts and Sciences.
In 2005, the CNDR researchers showed that the anti-cancer drug paclitaxel (Taxol™) could improve spinal cord nerve function in mice with tau tangles in their brains, after the drug was absorbed at nerve termini in muscle. “However, paclitaxel and related drugs do not cross the blood-brain barrier” notes Brunden. “So we surveyed a number of additional microtubule-stabilizing agents and discovered that the epothilone class, and in particular epothilone D, readily entered and persisted in the brain.”
“The positive effect of epothilone D on the function of axons and on cognition, without the onset of side-effects offers hope that this class of microtubule-stabilizing drugs could progress to testing in Alzheimer patients in the near future,” says Lee.
“There are very few tau-focused drugs in clinical trials now for Alzheimer’s disease,” says Trojanowski. “While we and others have urged that pharmaceutical companies should not put all of their eggs in one drug basket to ensure the highest likelihood of finding disease-modifying therapies for Alzheimer’s, we hope this successful mouse study of a tau drug will encourage more pharmaceutical companies to pursue programs on tau-focused drug discovery.”
Help from Sponges
The epothilones are microtubule-binding drugs derived from marine sponges and have been used as anti-cancer drugs because they prevent cells from dividing. They do this by keeping microtubules overly stabilized, which blocks cell division and causes cell death in rapidly dividing cells such as cancer cells. However, since nerve cells do not replicate or divide, they are immune to the toxic effects of microtubule-binding drugs.
In Alzheimer’s disease and other diseases with tau clumps in the brain, the hope is that a microtubule-stabilizing drug will restore the microtubule tracks to their original supportive structure. This led the researchers to give the tau mice epothilone D (epoD) to replace the now unavailable tau.
Indeed, epothilone D improved the brain function of tau mice, which have tau inclusions in their forebrain, degenerated axons, and broken microtubules. After treating three-month old male tau mice with a low dose of epoD once a week for three months, the mice showed increased numbers of microtubules and improved axon integrity, without notable side effects to organs and immune cells.
What’s more, epothilone D reduced deficits in memory and learning in the tau mice. “EpoD improves cognition in mice affected by neurodegenerative tau pathology. These findings suggest that epothilone D and other microtubule-stabilizing agents hold considerable promise as potential treatments for neurodegenerative diseases in humans,” says senior author Amos B. Smith III, PhD, the Rhodes Thompson Professor of Chemistry.
This research was funded by the National Institute on Aging and the Marian S. Ware Alzheimer Program.
Penn Medicine is one of the world’s leading academic medical centers, dedicated to the related missions of medical education, biomedical research, and excellence in patient care. Penn Medicine consists of the University of Pennsylvania School of Medicine (founded in 1765 as the nation's first medical school) and the University of Pennsylvania Health System, which together form a $3.6 billion enterprise.
Penn’s School of Medicine is currently ranked #2 in U.S. News & World Report’s survey of research-oriented medical schools, and is consistently among the nation’s top recipients of funding from the National Institutes of Health, with $367.2 million awarded in the 2008 fiscal year.
Penn Medicine’s patient care facilities include:
The Hospital of the University of Pennsylvania – the nation’s first teaching hospital, recognized as one of the nation’s top 10 hospitals by U.S. News & World Report.
Penn Presbyterian Medical Center – named one of the top 100 hospitals for cardiovascular care by Thomson Reuters for six years.
Pennsylvania Hospital – the nation’s first hospital, founded in 1751, nationally recognized for excellence in orthopaedics, obstetrics & gynecology, and psychiatry & behavioral health.
Additional patient care facilities and services include Penn Medicine at Rittenhouse, a Philadelphia campus offering inpatient rehabilitation and outpatient care in many specialties; as well as a primary care provider network; a faculty practice plan; home care and hospice services; and several multispecialty outpatient facilities across the Philadelphia region.
Penn Medicine is committed to improving lives and health through a variety of community-based programs and activities. In fiscal year 2009, Penn Medicine provided $733.5 million to benefit our community.
Media Contact
All latest news from the category: Life Sciences and Chemistry
Articles and reports from the Life Sciences and chemistry area deal with applied and basic research into modern biology, chemistry and human medicine.
Valuable information can be found on a range of life sciences fields including bacteriology, biochemistry, bionics, bioinformatics, biophysics, biotechnology, genetics, geobotany, human biology, marine biology, microbiology, molecular biology, cellular biology, zoology, bioinorganic chemistry, microchemistry and environmental chemistry.
Newest articles

Properties of new materials for microchips
… can now be measured well. Reseachers of Delft University of Technology demonstrated measuring performance properties of ultrathin silicon membranes. Making ever smaller and more powerful chips requires new ultrathin…

Floating solar’s potential
… to support sustainable development by addressing climate, water, and energy goals holistically. A new study published this week in Nature Energy raises the potential for floating solar photovoltaics (FPV)…
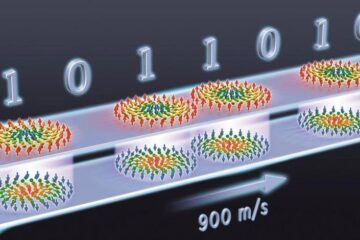
Skyrmions move at record speeds
… a step towards the computing of the future. An international research team led by scientists from the CNRS1 has discovered that the magnetic nanobubbles2 known as skyrmions can be…





















