Mass. General researchers isolate egg-producing stem cells from adult human ovaries

For the first time, Massachusetts General Hospital (MGH) researchers have isolated egg-producing stem cells from the ovaries of reproductive age women and shown these cells can produce what appear to be normal egg cells or oocytes. In the March issue of Nature Medicine, the team from the Vincent Center for Reproductive Biology at MGH reports the latest follow-up study to their now-landmark 2004 Nature paper that first suggested female mammals continue producing egg cells into adulthood.
“The primary objective of the current study was to prove that oocyte-producing stem cells do in fact exist in the ovaries of women during reproductive life, which we feel this study demonstrates very clearly,” says Jonathan Tilly, PhD, director of the Vincent Center for Reproductive Biology in the MGH Vincent Department of Obstetrics and Gynecology, who led the study. “The discovery of oocyte precursor cells in adult human ovaries, coupled with the fact that these cells share the same characteristic features of their mouse counterparts that produce fully functional eggs, opens the door for development of unprecedented technologies to overcome infertility in women and perhaps even delay the timing of ovarian failure.”
The 2004 report from Tilly's team challenged the fundamental belief, held since the 1950s, that female mammals are born with a finite supply of eggs that is depleted throughout life and exhausted at menopause. That paper and a 2005 follow-up published in Cell showing that bone marrow or blood cell transplants could restore oocyte production in adult female mice after fertility-destroying chemotherapy were controversial; but in the intervening years, several studies from the MGH-Vincent group and other researchers around the world have supported Tilly's work and conclusions.
These supporting studies include a 2007 Journal of Clinical Oncology report from the MGH-Vincent team that showed female mice receiving bone marrow transplants after oocyte-destroying chemotherapy were able to have successful pregnancies, delivering pups that were their genetic offspring and not of the marrow donors. A 2009 study from a team at Shanghai Jiao Tong University in China, published in Nature Cell Biology, not only isolated and cultured oocyte-producing stem cells (OSCs) from adult mice but also showed that those OSCs, after transplantation into the ovaries of chemotherapy-treated female mice, gave rise to mature oocytes that were ovulated, fertilized and developed into healthy offspring.
“That study singlehandedly deflated many of the arguments from critics of our earlier Nature paper by showing that oocyte-producing stem cells exist in mice and could develop into fully functional eggs,” says Tilly. Another paper from a west-coast biotechnology company, published in Differentiation in 2010, provided further independent confirmation of Tilly's earlier conclusions regarding the presence of oocyte-producing stem cells in ovaries of adult mice.
Tilly is quick to point out, however, “These follow-up studies, while providing definitive evidence that oocyte-producing stem cells exist in ovaries of adult female mammals, were not without their limitations, leaving the question open in some scientific circles of whether the adult oocyte pool can be renewed. For example, the protocol used to isolate OSCs in the 2009 Nature Cell Biology study is a relatively crude approach that often results in the contamination of desired cells by other cell types.” To address this, the MGH-Vincent team developed and validated a much more precise cell-sorting technique to isolate OSCs without contamination from other cells.
The 2009 study from China also had isolated OSCs based on cell-surface expression of a marker protein called Ddx4 or Mvh, which previously had been found only in the cytoplasm of oocytes. This apparent contradiction with earlier studies raised concerns over the validity of the protocol. Using their state-of-the-art fluorescence-activated cell sorting techniques, the MGH-Vincent team verified that, while the marker protein Ddx4 was indeed located inside oocytes, it was expressed on the surface of a rare and distinct population of ovarian cells identified by numerous genetic markers and functional tests as OSCs.
To examine the functional capabilities of the cells isolated with their new protocol, the investigators injected green fluorescent protein (GFP)-labeled mouse OSCs into the ovaries of normal adult mice. Several months later, examination of the recipient mouse ovaries revealed follicles containing oocytes with and without the marker protein. GFP-labeled and unlabeled oocytes also were found in cell clusters flushed from the animals' oviducts after induced ovulation. The GFP-labeled mouse eggs retrieved from the oviducts were successfully fertilized in vitro and produced embryos that progressed to the hatching blastocyst stage, a sign of normal developmental potential. Additionally, although the Chinese team had transplanted OSCs into ovaries of mice previously treated with chemotherapy, the MGH-Vincent team showed that it was not necessary to damage the recipient mouse ovaries with toxic drugs before introducing OSCs.
In their last two experiments, which Tilly considers to be the most groundbreaking, the MGH-Vincent team used their new cell-sorting techniques to isolate potential OSCs from adult human ovaries. The cells obtained shared all of the genetic and growth properties of the equivalent cells isolated from adult mouse ovaries, and like mouse OSCs, were able to spontaneously form cells with characteristic features of oocytes. Not only did these oocytes formed in culture dishes have the physical appearance and gene expression patterns of oocytes seen in human ovaries – as was the case in parallel mouse experiments – but some of these in-vitro-formed cells had only half of the genetic material normally found in all other cells of the body. That observation indicates that these oocytes had progressed through meiosis, a cell-division process unique to the formation of mature eggs and sperm.
The researchers next injected GFP-labeled human OSCs into biopsied human ovarian tissue that was then grafted beneath the skin of immune-system-deficient mice. Examination of the human tissue grafts 7 to 14 days later revealed immature human follicles with GFP-negative oocytes, probably present in the human tissue before OSC injection and grafting, as well as numerous immature human follicles with GFP-positive oocytes that would have originated from the injected human OSCs.
“These experiments provide pivotal proof-of-concept that human OSCs reintroduced into adult human ovarian tissue performed their expected function of generating new oocytes that become enclosed by host cells to form new follicles,” says Tilly, a professor of Obstetrics, Gynecology and Reproductive Biology at Harvard Medical School and chief of Research at the MGH Vincent Department of Obstetrics and Gynecology. “These outcomes are exactly what we see if we perform the same experiments using GFP-expressing mouse OSCs, and GFP-expressing mouse oocytes formed that way go on to develop into fully functional eggs.
“In this paper we provide the three key pieces of evidence requested by those who have been skeptical of our previous work,” he adds. “We developed and extensively validated a cell-sorting protocol to reliably purify OSCs from adult mammalian ovaries, proving once again that these very special cells exist. We tested the function of mouse oocytes produced by these OSCs and showed that they can be fertilized to produce healthy embryos. And we identified and characterized an equivalent population of oocyte-producing stem cells isolated from adult human ovaries.”
Among the many potential clinical applications for these findings that Tilly's team is currently exploring are the establishment of human OSC banks – since these cells, unlike human oocytes, can be frozen and thawed without damage – the identification of hormones and factors that accelerate the formation of oocytes from human OSCs, the development of mature human oocytes from OSCs for in vitro fertilization, and other approaches to improve the outcomes of IVF and other infertility treatments.
Tilly notes that an essential part of his group's accomplishment was collaboration with study co-author Yasushi Takai, MD, PhD, a former MGH research fellow on Tilly's team and now a faculty member at Saitama Medical University in Japan. Working with his clinical colleagues at Saitama, Takai was able to provide healthy ovarian tissue from consenting patients undergoing sex reassignment surgery, many in their 20s and early 30s. Co-lead authors of the Nature Medicine report are Yvonne White, PhD, and Dori Woods, PhD, of the Vincent Center for Reproductive Biology at MGH. Additional co-authors are Osamu Ishihara, MD, PhD, and Hiroyuki Seki, MD, PhD, of Saitama Medical University.
The study was supported by a 10-year MERIT Award to Tilly from the National Institute on Aging, a Ruth L. Kirschstein National Research Service Award from the National Institutes of Health, the Henry and Vivian Rosenberg Philanthropic Fund, the Sea Breeze Foundation, and Vincent Memorial Hospital Research Funds. Tilly is a co-founder of OvaScience, Inc. (www.ovascience.com), which has licensed the commercial potential of these and other patent-protected findings of the MGH-Vincent team for development of new fertility-enhancing procedures.
Massachusetts General Hospital (www.massgeneral.org), founded in 1811, is the original and largest teaching hospital of Harvard Medical School. The MGH conducts the largest hospital-based research program in the United States, with an annual research budget of more than $750 million and major research centers in AIDS, cardiovascular research, cancer, computational and integrative biology, cutaneous biology, human genetics, medical imaging, neurodegenerative disorders, regenerative medicine, reproductive biology, systems biology, transplantation biology and photomedicine.
Media Contact
More Information:
http://www.massgeneral.orgAll latest news from the category: Life Sciences and Chemistry
Articles and reports from the Life Sciences and chemistry area deal with applied and basic research into modern biology, chemistry and human medicine.
Valuable information can be found on a range of life sciences fields including bacteriology, biochemistry, bionics, bioinformatics, biophysics, biotechnology, genetics, geobotany, human biology, marine biology, microbiology, molecular biology, cellular biology, zoology, bioinorganic chemistry, microchemistry and environmental chemistry.
Newest articles
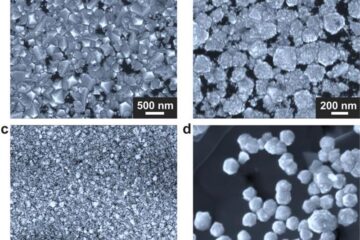
Making diamonds at ambient pressure
Scientists develop novel liquid metal alloy system to synthesize diamond under moderate conditions. Did you know that 99% of synthetic diamonds are currently produced using high-pressure and high-temperature (HPHT) methods?[2]…
Eruption of mega-magnetic star lights up nearby galaxy
Thanks to ESA satellites, an international team including UNIGE researchers has detected a giant eruption coming from a magnetar, an extremely magnetic neutron star. While ESA’s satellite INTEGRAL was observing…
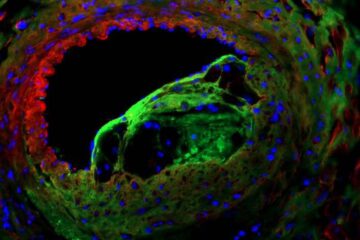
Solving the riddle of the sphingolipids in coronary artery disease
Weill Cornell Medicine investigators have uncovered a way to unleash in blood vessels the protective effects of a type of fat-related molecule known as a sphingolipid, suggesting a promising new…





















