How Insulin in the Brain May Suppress the Subjective Feeling of Hunger
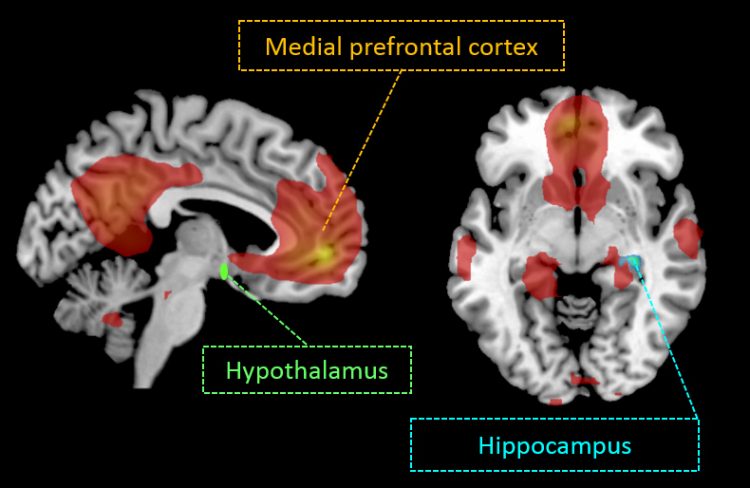
Intranasal insulin enhances functional connectivity in specific cognitive brain regions (default-mode network, DMN) as well as in the hippocampus and the hypothalamus. Image source: IDM
Eating behavior and the subjective feeling of hunger are regulated by a variety of hormones. Here a key role is played by the hormone insulin because it is not only active in the body, but also in the brain. It was previously known that insulin acts on the homeostatic region (hypothalamus**).
Now, however, scientists have found that the hormone is also active in other brain regions. Researchers at the Institute for Diabetes Research and Metabolic Diseases of Helmholtz Zentrum München at the University of Tübingen, a partner of the DZD, have further deciphered the function of insulin in the brain as well as its influence on the subjective feeling of hunger and have published their findings in Scientific Reports, a Nature research journal.
To better understand the mechanism of action of insulin, the researchers administered insulin intranasally to healthy young adults. Through the application of the hormone via a nasal spray, the blood-brain barrier is bypassed and the insulin reaches the brain directly. In the study, 25 lean, ten overweight and 12 obese participants “sniffed” insulin or the placebo. Brain activity was then visualized and recorded by means of a functional magnetic resonance imaging (fMRI) scan.
The result in all study participants: Intranasal insulin improves functional connectivity in the prefrontal regions of the default-mode network (DMN), a group of brain regions that are activated when a person is at rest and is not performing any tasks. This region is central to cognitive processes. In addition, the functional connectivity between the DMN and the hippocampus as well as the hypothalamus is strengthened.
These changes in the brain also influence eating behavior and alter the relationship between adiposity and the hunger sensation. Actually, people with a lot of visceral adipose tissue*** have an increased sensation of hunger. “Insulin-enhanced connectivity between the DMN and the hippocampus suppresses the relationship between adipose tissue and the subjective hunger feeling,” said Stephanie Kullmann, author of the study. The study participants felt less hunger after being administered intranasal insulin.
In addition, the scientists observed that insulin in the brain also improves the effect of the hormone in the body. Study participants with insulin-induced increased functional connectivity in the DMN have higher insulin sensitivity in the body. This counteracts obesity and type 2 diabetes.
The current results show that insulin in the brain – due to increased functional connectivity between cognitive and homeostatic regions – may help regulate eating behavior and facilitate weight loss.
Original Publication:
Stephanie Kullmann, Martin Heni, Ralf Veit, Klaus Scheffler, Jürgen Machann, Hans-Ulrich Häring, Andreas Fritsche, Hubert Preissl. Intranasal insulin enhances brain functional connectivity mediating the relationship between adiposity and subjective feeling of hunger. Scientific Reports | 7: 1627 | DOI:10.1038/s41598-017-01907-w
* The default-mode network DMN is a group of brain regions that is active when a person is daydreaming, making future plans, etc. It enables thinking without having a stimulus.
** The hypothalamus is the supreme regulatory center for all vegetative and endocrine processes. The hypothalamus coordinates water and saline balance as well as blood pressure. It ensures the maintenance of the inner milieu (homeostasis) and regulates food intake.
*** The fatty tissue on and especially in the abdomen is called visceral fat. It is stored in the free abdominal cavity and envelops the internal organs – especially the organs of the digestive system. There is a relationship between visceral adipose tissue and the subjective feeling of hunger.
Scientific Contact:
Dr. Stephanie Kullmann
Institute for Diabetes Research and Metabolic Diseases (IDM)
of Helmholtz Zentrum München at the University of Tübingen
Otfried-Müller-Straße 47
72076 Tübingen
Germany
Phone: +49 (0)7071-2987703
email: stephanie.kullmann@med.uni-tuebingen.de
Media Contact:
Birgit Niesing
German Center for Diabetes Research (DZD
Ingolstädter Landstraße 1
85764 Neuherberg
Germany
Phone: +49 (0)89-3187-3971
email: niesing@dzd-ev.de
The German Center for Diabetes Research (DZD) is one of six German Centers for Health Research. It brings together experts in the field of diabetes research and integrates basic research, epidemiology, and clinical applications. By adopting an innovative, integrative approach to research, the DZD aims to make a substantial contribution to the successful personalized prevention diagnosis and treatment of diabetes mellitus. The members of the DZD are Helmholtz Zentrum München – German Research Center for Environmental Health, the German Diabetes Center (DDZ) in Düsseldorf, the German Institute of Human Nutrition (DIfE) in Potsdam-Rehbrücke, the Institute of Diabetes Research and Metabolic Diseases of Helmholtz Zentrum München at the University of Tübingen, the Paul Langerhans Institute Dresden of Helmholtz Zentrum München at the Carl Gustav Carus University Hospital of TU Dresden, associated partners at the universities in Heidelberg, Cologne, Leipzig, Lübeck and Munich, and other project partners. www.dzd-ev.de
The Helmholtz Zentrum München, the German Research Center for Environmental Health, pursues the goal of developing personalized medical approaches for the prevention and therapy of major common diseases such as diabetes and lung diseases. To achieve this, it investigates the interaction of genetics, environmental factors and lifestyle. The Helmholtz Zentrum München is headquartered in Neuherberg in the north of Munich and has about 2,300 staff members. It is a member of the Helmholtz Association, a community of 18 scientific-technical and medical-biological research centers with a total of about 37,000 staff members. www.helmholtz-muenchen.de/en
Media Contact
All latest news from the category: Life Sciences and Chemistry
Articles and reports from the Life Sciences and chemistry area deal with applied and basic research into modern biology, chemistry and human medicine.
Valuable information can be found on a range of life sciences fields including bacteriology, biochemistry, bionics, bioinformatics, biophysics, biotechnology, genetics, geobotany, human biology, marine biology, microbiology, molecular biology, cellular biology, zoology, bioinorganic chemistry, microchemistry and environmental chemistry.
Newest articles

Properties of new materials for microchips
… can now be measured well. Reseachers of Delft University of Technology demonstrated measuring performance properties of ultrathin silicon membranes. Making ever smaller and more powerful chips requires new ultrathin…

Floating solar’s potential
… to support sustainable development by addressing climate, water, and energy goals holistically. A new study published this week in Nature Energy raises the potential for floating solar photovoltaics (FPV)…
Skyrmions move at record speeds
… a step towards the computing of the future. An international research team led by scientists from the CNRS1 has discovered that the magnetic nanobubbles2 known as skyrmions can be…





















