Glutamate:Too Much of a Good Thing in Schizophrenia?

While the predominant hypothesis for many years was that schizophrenia was a glutamate deficit disorder, there is growing evidence of glutamate hyperactivity as well. The study by Karlsson et al., appearing in the November 1st issue of Biological Psychiatry, reinforces this point with new data about the impact of deleting the gene for the glutamate transporter EAAT1.
EAAT1, implicated in schizophrenia, plays a critical role in inactivating glutamate by removing it from the synaptic and extracellular spaces. The authors demonstrate that these “knockout” animals show increased responses to the NMDA glutamate receptor antagonist, MK-801. This drug causes the release of more glutamate into the synapse in the frontal cortex. This effect of MK-801 is reduced by a group II metabotropic glutamate receptor agonist, which reduces glutamate release.
Dr. Andrew Holmes, corresponding author, further discusses their findings, “Our study adds a new twist to [glutamate] research by showing that genetically disrupting a major regulator of glutamate’s ability to communicate between nerve cells produces certain ‘schizophrenia-like’ features in mice and, moreover, that these abnormalities can be corrected by a highly promising new class of glutamate-targeting antipsychotic treatments.” In fact, this class of drugs has already shown some preliminary efficacy in its ability to treat individuals suffering from schizophrenia.
John H. Krystal, M.D., Editor of Biological Psychiatry and affiliated with both Yale University School of Medicine and the VA Connecticut Healthcare System, comments: “The NMDA receptor antagonist model and the EAAT1 knockout animal push us to take a fresh look at the obstacles to treating cognitive impairments associated with schizophrenia, in other words, optimizing their cortical network function. This new look can lead us to drugs that would have been completely surprising as recently as 10 years ago, such as the group II metabotropic glutamate receptor agonists.”
Dr. Holmes does note that further research is warranted, stating, “What is now needed is more research to get a better handle on how disrupting this gene affects the brain’s neural wiring and molecular signaling pathways to produce the symptoms of schizophrenia.” This finding could ultimately help scientists develop new or improved treatments for this schizophrenia.
Media Contact
More Information:
http://www.elsevier.comAll latest news from the category: Health and Medicine
This subject area encompasses research and studies in the field of human medicine.
Among the wide-ranging list of topics covered here are anesthesiology, anatomy, surgery, human genetics, hygiene and environmental medicine, internal medicine, neurology, pharmacology, physiology, urology and dental medicine.
Newest articles

Combatting disruptive ‘noise’ in quantum communication
In a significant milestone for quantum communication technology, an experiment has demonstrated how networks can be leveraged to combat disruptive ‘noise’ in quantum communications. The international effort led by researchers…
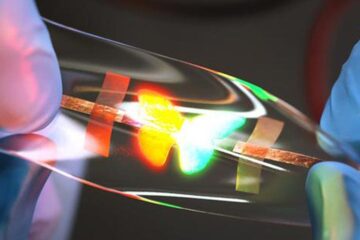
Stretchable quantum dot display
Intrinsically stretchable quantum dot-based light-emitting diodes achieved record-breaking performance. A team of South Korean scientists led by Professor KIM Dae-Hyeong of the Center for Nanoparticle Research within the Institute for…

Internet can achieve quantum speed with light saved as sound
Researchers at the University of Copenhagen’s Niels Bohr Institute have developed a new way to create quantum memory: A small drum can store data sent with light in its sonic…





















